Epilepsy is one of the most frequent chronic neurological disorders. In 30 to 40% of the patients, seizures cannot be controlled adequately with medication, whose cases are called drug-resistant epilepsy. For 10 to 50% of these patients, surgery constitutes a valuable treatment option. Aims of the surgery is to control seizures by resection of the epileptogenic tissue without causing damage to areas of the brain responsible for essential functions. Candidates for lesionectomy undergo an extensive pre-surgery evaluation. Magnetic resonance imaging (MRI) is of paramount importance in this presurgical evaluation to detect and delineate lesions. Detection of a previously undetected lesion can drastically change the presurgical planning and significantly improve seizure post-surgery outcome. Yet some kind of lesions, as subtle focal cortical dysplasia (FCD), are more difficult to detect because of their small sizes, and often buried in the complex convexities of the cortex. Practical constraints of time may lead MRI readers to miss those lesions that require increased scrutiny.
In a prospective trial, Professor Riem El Tahry & Professor Susana Ferrao santos (Center for Refractory Epilepsy, Cliniques Universitaires Saint-Luc), evaluated the detection rate of a voxel-based MRI morphometric analysis program (MAP), implemented based on algorithms of the open source statistical parametric mapping (SPM) software developed by H.-J. Huppertz1, to facilitate the detection of FCD. MAP directs the reader’s attention to suspicious brain regions, on the basis of features commonly accompanying FCD, i.e., abnormal gray‐white junction blurring, abnormal cortical gyration, or abnormal cortical thickness.
They studied the positive (MAP+) surgical candidates results findings in terms of their clinical value in the decision-making process of the presurgical evaluation. 21 patients who had negative MRI by visual analysis were included prospectively. In a first step, results of the conventional non-invasive presurgical evaluation were discussed blinded to the MAP results in multidisciplinary epilepsy surgery meetings to determine the possible seizure onset zone and to set surgical or invasive evaluation plans. Thereafter, MAP results were presented and the change of initial clinical plan was studied. All MAP detections were viewed by a neuroradiologist with epilepsy expertise. For the 21 patients included (4 with temporal lobe epilepsy and 17 with extra temporal lobe epilepsy), MAP was positive in 10/21 (47%) patients and in 6/10 (60%) a diagnosis of focal cortical dysplasia was confirmed after review, corresponding to a 28% detection rate. MAP+ findings had a clear impact on the initial management in 7/10 patients (7/21, 33% of all patients), which included an adaptation of the intracranial EEG plan (6/7), or the decision to proceed directly to surgery (1/7). MRI post-processing technique thus appears to be of essential help in order to optimize the detection of subtle lesions that might escape conventional visual analysis even with high‐resolution dedicated epilepsy MRI protocols reviewed by expert neuroradiologists.
R. El Tahry & S. Ferrao santos. Center for Refractory Epilepsy, Cliniques Universitaires Saint-Luc.
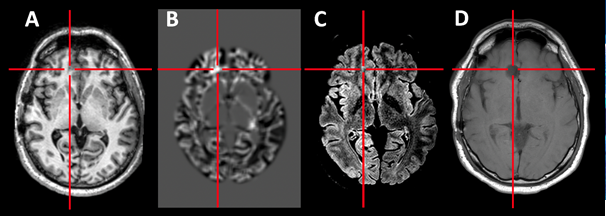
Figure 1 : In patient 21, the MAP+ region confirmed the initial hypothesis of a left mesial frontal seizure onset zone. Therefore, the patient did not go through intracranial EEG and a resection was proposed after repeating the MRI, which confirmed the lesion. The patient became seizure free.
1Huppertz, H.J., Grimm, C., Fauser, S. , et al. 2005. Enhanced visualization of blurred gray-white matter junctions in focal cortical dysplasia by voxel-based 3D MRI analysis. Epilepsy Res.2005;67(1-2):35-50
